Barrett’s Esophagus represents a significant concern in gastrointestinal health, stemming from the more commonly encountered Gastroesophageal Reflux Disease (GERD). Understanding the intricacies of this condition is crucial for effective management and prevention. This blog post delves into the symptoms, causes, and preventive measures of Barrett’s Esophagus, offering insights for those affected and at risk.
What is Barrett’s Esophagus?
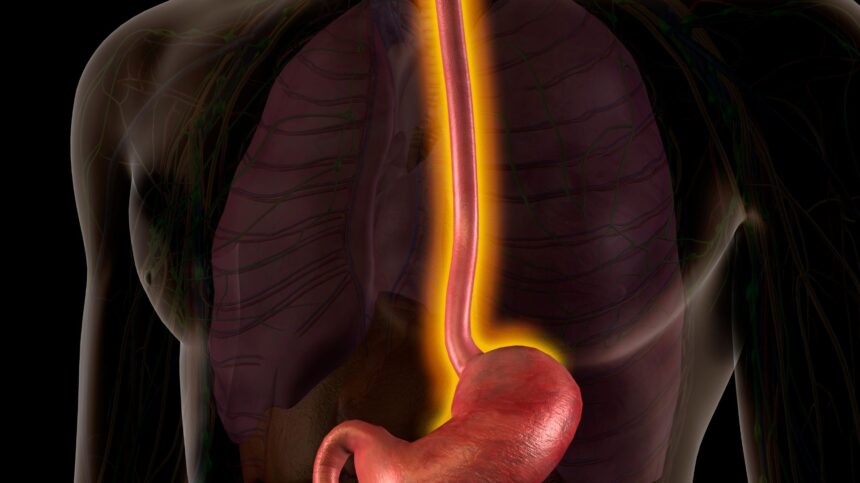
Barrett’s Esophagus is a condition where the lining of the esophagus undergoes a transformation, typically due to prolonged exposure to stomach acid. This acid reflux damages the inner lining, leading to the replacement of the normal esophageal cells with specialized columnar cells. Such cellular changes not only cause discomfort but also elevate the risk of developing esophageal cancer, albeit in rare instances.
GERD: The Primary Culprit
The exact causes of Barrett’s Esophagus remain under investigation, but the link with GERD is undeniable. GERD arises when the esophagus is damaged by stomach acids over time, influenced by factors such as diet, lifestyle, obesity, and physical inactivity. Symptoms like persistent heartburn or chest pain significantly increase the risk of Barrett’s Esophagus, highlighting the need for medical consultation for those experiencing such signs.
Recognizing the Symptoms
Barrett’s Esophagus shares many symptoms with GERD, making early detection challenging. Key symptoms include:
- Persistent chest pain and heartburn
- Nausea, vomiting, and throat pain
- Difficulty swallowing and breathing
- Regurgitation of food
- An unpleasant, sour taste in the mouth and increased saliva production
Who Is at Risk?
Certain factors increase the likelihood of developing Barrett’s Esophagus:
- Age: It’s more common in older adults.
- Gender: Men are at higher risk, though women are also affected.
- Obesity: Excess weight significantly contributes to the risk.
- Lifestyle: Consumption of spicy foods, red meat, smoking, and alcoholism are key risk factors.
Complications
If untreated, Barrett’s Esophagus can lead to serious complications, including:
- Stricture: Narrowing of the esophagus due to damage, leading to swallowing difficulties.
- Esophageal Sores: Ulcers caused by acid damage.
- Dysplasia: Precancerous changes in the esophageal cells.
Treatment Options
Diagnosis typically involves endoscopy and, if necessary, a biopsy. Treatment aligns with the severity of the condition and can range from medication to manage GERD to more invasive procedures to address severe dysplasia.
Prevention: A Proactive Approach
While Barrett’s Esophagus itself is irreversible, proactive measures can mitigate risk factors:
- Dietary Changes: Adopting a healthy diet low in acidic and spicy foods.
- Weight Management: Maintaining a healthy body weight.
- Lifestyle Adjustments: Quitting smoking and reducing alcohol consumption.
- Managing GERD: Early treatment of GERD can prevent its progression to Barrett’s Esophagus.
Conclusion
Barrett’s Esophagus, a serious condition resulting from untreated GERD, underscores the importance of lifestyle and dietary choices in gastrointestinal health. Recognizing symptoms early, understanding the risk factors, and adopting preventive measures are key steps in managing and mitigating its impact. For those at risk or experiencing symptoms, consulting a gastroenterologist is crucial for diagnosis and treatment, paving the way for a healthier esophageal condition.